Reclaiming Your Liver Health: A Guide to Fatty Liver Detoxification with Hemlock Pharmacy
The liver, our body’s unsung hero, tirelessly performs over 500 essential functions to keep us healthy. One of its primary roles is to filter toxins and waste products from our bloodstream. However, unhealthy lifestyle choices can overburden the liver, leading to a condition called fatty liver disease (FLD). This article will delve into FLD, explore natural detoxification methods, and introduce Hemlock Pharmacy’s range of products that can support your journey towards a healthier liver.
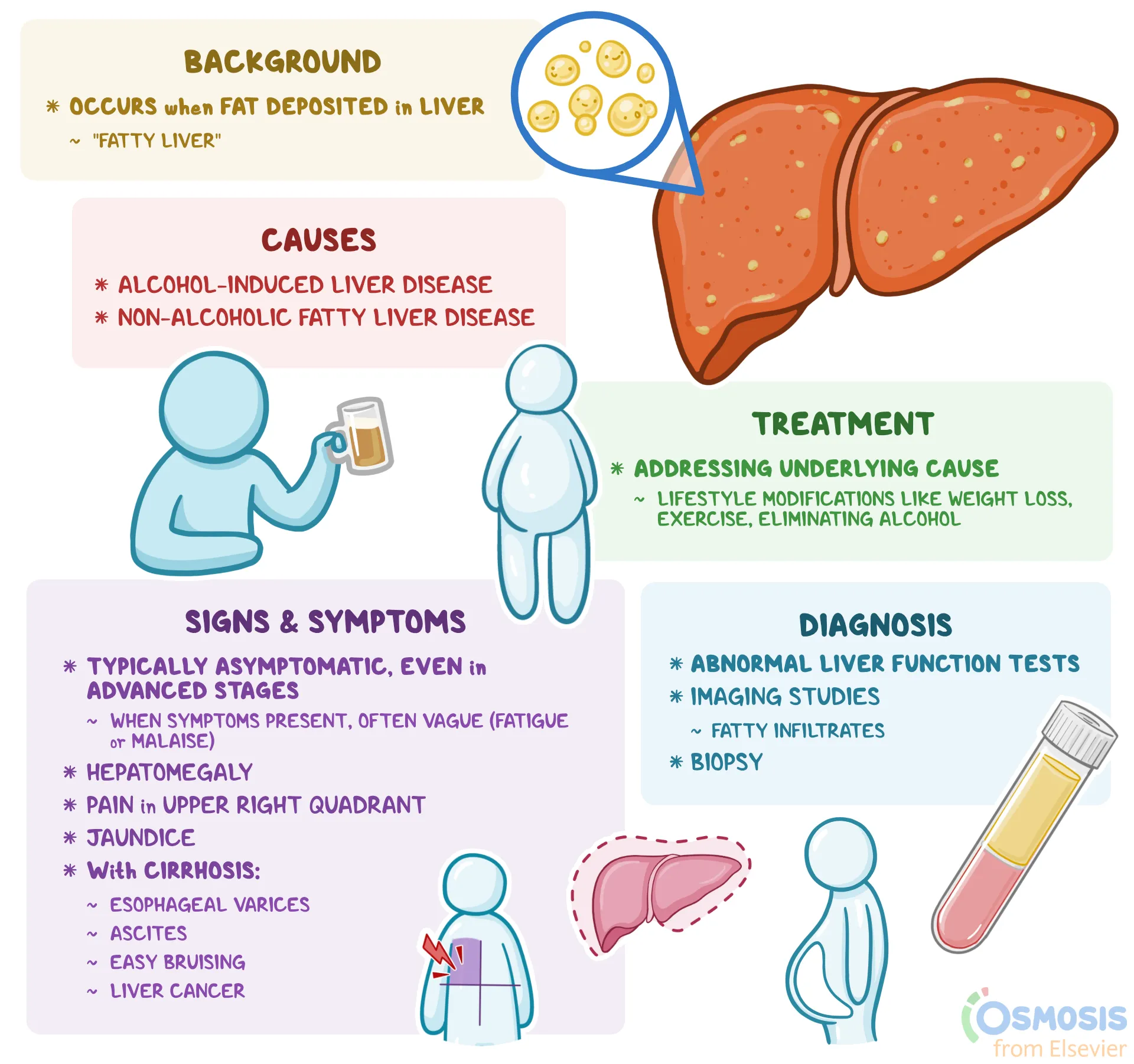
Understanding Fatty Liver Disease
FLD is a spectrum of liver conditions characterized by an excessive buildup of fat in the liver cells. It can range from simple steatosis (fatty liver) to more severe forms like nonalcoholic steatohepatitis (NASH), which can lead to inflammation and scarring. While excessive alcohol consumption is a known risk factor, nonalcoholic fatty liver disease (NAFLD) is becoming increasingly prevalent, affecting millions globally.
Risk Factors for Fatty Liver Disease
Several factors can contribute to the development of FLD, including:
- Obesity and overweight: Excess body fat, particularly visceral fat around the abdomen, increases the risk of FLD.
- Insulin resistance: When the body struggles to utilize insulin effectively, it can lead to fat accumulation in the liver.
- Metabolic syndrome: A cluster of conditions including high blood pressure, high blood sugar, and unhealthy cholesterol levels, significantly increases the risk of FLD.
- Diet: A diet high in saturated fats, sugary drinks, and refined carbohydrates can contribute to FLD.
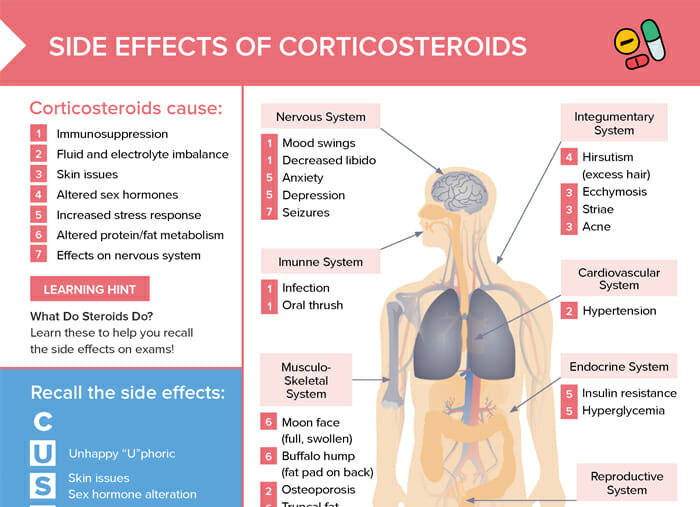
- Certain medications: Some medications can have side effects that lead to fat accumulation in the liver.
Symptoms of Fatty Liver Disease
FLD often progresses silently without any noticeable symptoms. However, in some cases, individuals may experience:
- Fatigue
- Loss of appetite
- Unexplained weight loss
- Upper right abdominal pain or discomfort
The Importance of Liver Detoxification
The liver naturally detoxifies our bodies. However, unhealthy lifestyle habits can compromise its ability to function optimally. Liver detoxification aims to support the liver’s natural cleansing processes, promoting overall well-being.
Natural Approaches to Fatty Liver Detoxification
Several natural strategies can support your liver’s detoxification process:
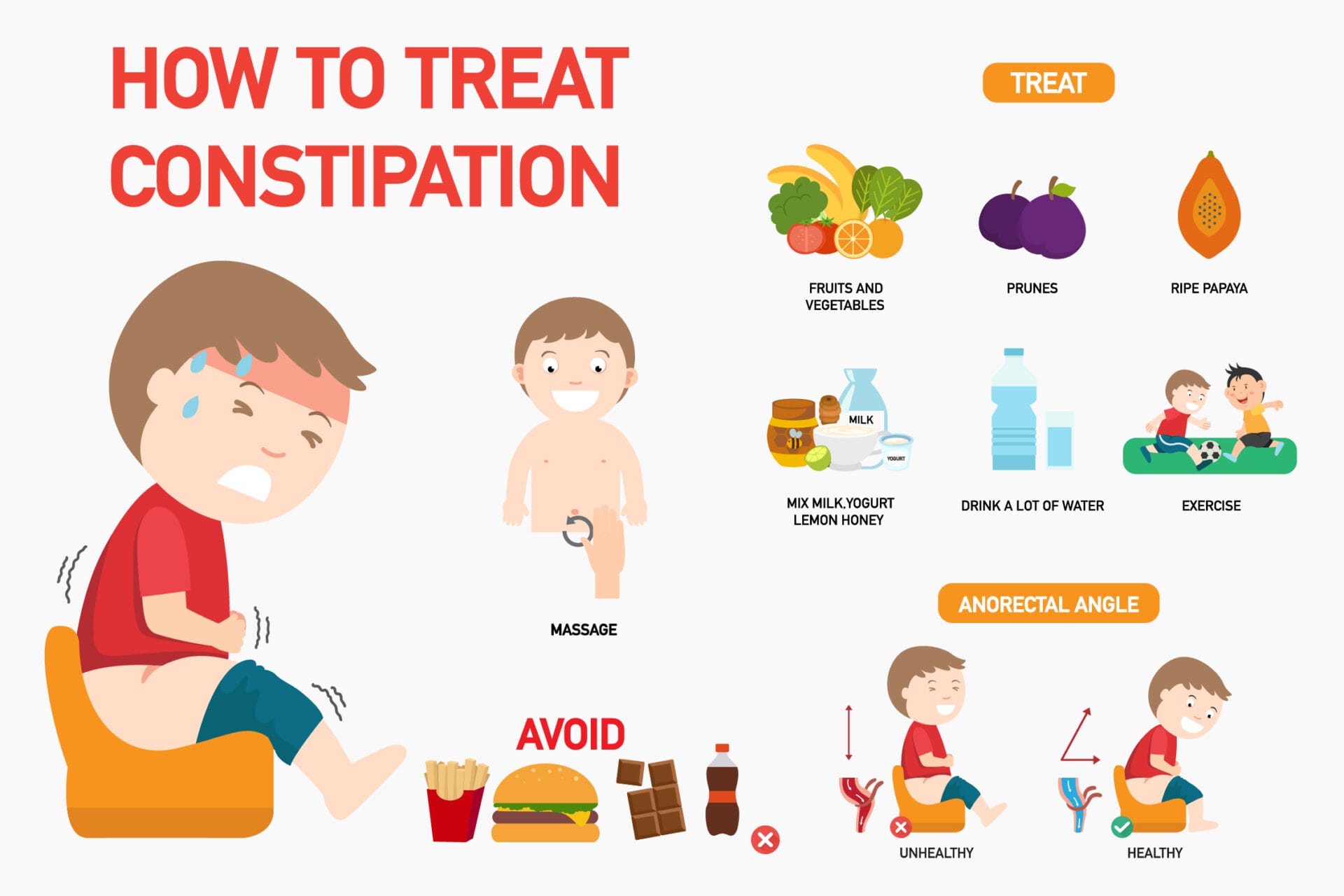
- Dietary Changes: Shifting towards a balanced diet rich in fruits, vegetables, whole grains, and lean protein can significantly improve liver health. Limiting saturated fats, processed foods, and sugary drinks is crucial.
- Exercise: Regular physical activity helps manage weight and improve insulin sensitivity, both beneficial for liver health.
- Weight Management: Losing weight, even a modest amount, can significantly improve liver function in individuals with FLD.
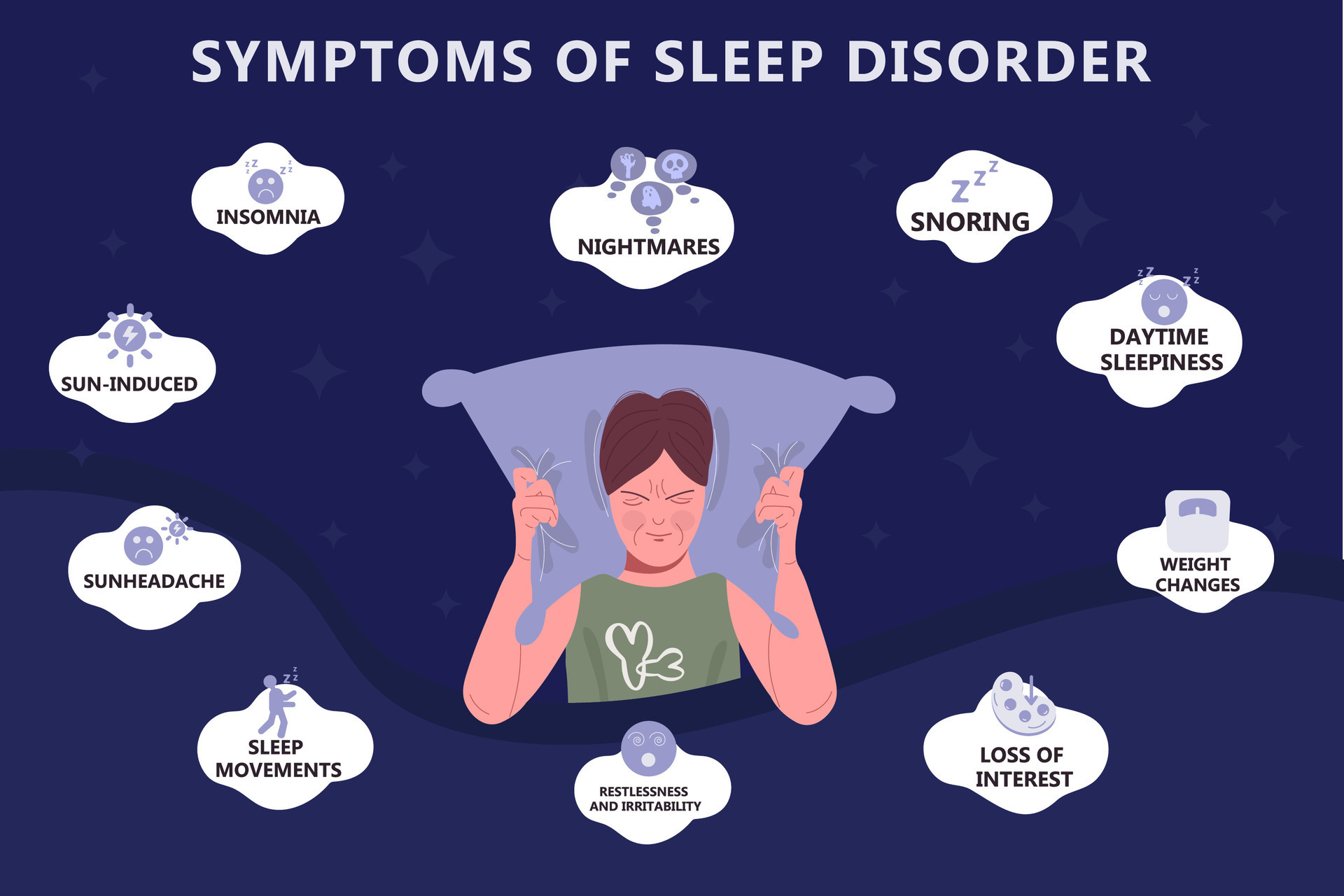
- Adequate Sleep: Aim for 7-8 hours of quality sleep each night to allow the liver time to repair and regenerate.
- Stress Management: Chronic stress can negatively impact liver health. Techniques like meditation, yoga, or deep breathing can be helpful.
Hemlock Pharmacy: Your Partner in Liver Health
Hemlock Pharmacy understands the importance of a healthy liver. They offer a range of natural products that can effectively support your liver detoxification journey:
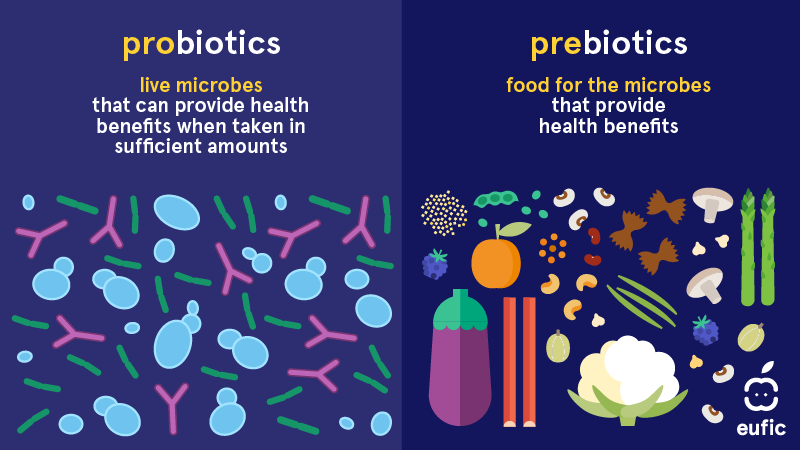
- Milk Thistle: A well-researched herb with silymarin, a potent antioxidant and anti-inflammatory compound that protects liver cells and promotes regeneration.
- Dandelion Root: A natural diuretic that helps eliminate toxins and excess fluids from the body, reducing stress on the liver.
- N-Acetyl Cysteine (NAC): An amino acid that supports glutathione production, the body’s master antioxidant, crucial for detoxification processes.
- Turmeric: Curcumin, the active compound in turmeric, has potent anti-inflammatory and antioxidant properties that can benefit liver health.
- B Vitamins: Play a vital role in liver function and metabolism. Vitamin B complex supplements can be helpful, especially for individuals with deficiencies.
Remember: It’s vital to consult with a healthcare professional before starting any new supplements, especially if you have underlying health conditions or take medications. They can advise on the appropriate dosage and potential interactions.
Conclusion
Fatty liver disease is a growing concern, but with early intervention and lifestyle modifications, it can be effectively managed. Hemlock Pharmacy’s natural product range, coupled with a commitment to healthy habits, can empower you to reclaim your liver health and optimize your overall well-being.